Advocacy & Position Statements
2026
-
On behalf of the undersigned emergency medicine organizations, we would like to express our appreciation for the ACGME’s thoughtful and deliberate approach to the proposed Emergency Medicine Program Requirements. We recognize the significance of these decisions and the care required in their evaluation.
However, the absence of a decision and a clearly articulated timeline has created substantial challenges for both training programs and trainees. Program leaders must make strategic decisions related to recruitment, resource and time allocation, curriculum design, and institutional planning well in advance. Without clarity regarding the anticipated timeline and process, responsible long-term planning is impossible.
-
Our emergency medicine community has been closely following the ACGME’s deliberations regarding potential revisions to the Emergency Medicine Program requirements. We recognize this period of uncertainty and the recent decision to defer action can be challenging and, for many, adds to the existing pressures faced daily in our Emergency Departments.We also recognize the varied perspectives on the future of training in our specialty, which reflect our deep commitment and pride in Emergency Medicine.
-
CORD recognizes that recent events unfolding across the country, including those in Minnesota, have a real impact on the communities where our members live and work. For those in emergency medicine, these moments may further intensify the already significant demands of the profession including the emotional and moral strain associated with caring for individuals and communities affected by violence, fear, and uncertainty.
2025
-
With the public comment period for the proposed ACGME Program Requirements now closed, our emergency medicine organizations come together in a shared purpose to acknowledge this pivotal moment for emergency medicine education—and to reaffirm our commitment to the community we serve.
This process has surfaced divergent perspectives, and thoughtful feedback from across the specialty. While views differ on the potential impact of the proposed changes including a standardized four-year training structure, what remains unmistakably clear is our collective investment in the future of our programs, trainees, and profession.
-
An Update from CORD on the ACGME Proposed Changes
Over the past several weeks and months, in meetings, town halls, and other forums, we have heard from many of you—directly and passionately—about the proposed ACGME Program Requirements and your experience with the process. One message has come through clearly: many of you have not felt adequately supported by the Board during this critical comment period. Some felt unheard. Others felt uncertain about where CORD stood or what steps were being taken.
We are sincerely grateful to those of you who spoke up, organized your communities, submitted comments, and asked the hard questions—not only of the ACGME, but of us who represent you in our organization.
-
CORD’s Response to Proposed ACGME Changes
Now that the public comment period has closed for the proposed ACGME Program Requirements, we want to offer our reflections on where we’ve been—and where we must go together. We know this moment has stirred strong and deeply held beliefs that are challenging. For many, the proposed changes, especially the possibility of a required four-year training structure, feel like a threat to the identity, autonomy, and legacy of programs built with pride and purpose.
We want to say this directly: We recognize how difficult this process has been, and we honor the remarkable work that ALL programs have done for decades.
-

2025 EM Match
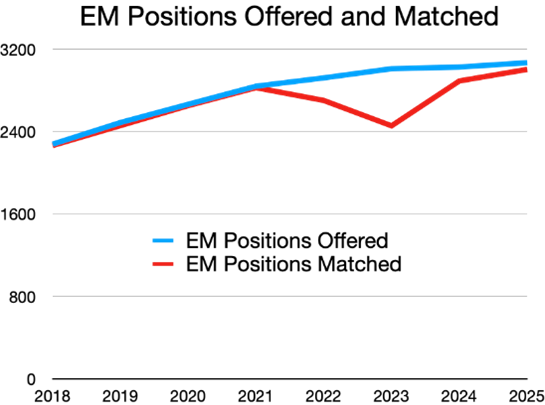
Thank you to everyone involved in making the 2025 EM Match a success! Between the hours recruiting, educating, and reviewing applicants to EM, it has been amazing to watch the EM family of organizations and individuals come together in this effort. This year we excitedly welcomed over 3000 new residents to Emergency Medicine
Together, we strive to make Emergency Medicine the best specialty in the House of Medicine. We welcome our new group of residents as they embark on their journey to fulfill their calling of “Anyone, Anything, Anytime.”
-
CORD’s Response to Proposed ACGME Changes
Thank you for your messages, emails, calls, and conversations regarding the proposed changes to the ACGME Program Requirements. We recognize the significant impact these changes could have on emergency medicine training programs, institutions, and our specialty. We want to clearly acknowledge the concerns, particularly surrounding the proposal for a universal four-year training format. We also hear the call for a more structured organizational response from CORD and want to provide the following statement:
2024
-
Statement on ResidencyCAS
Thank you all for your engagement and input at the CORD@ACEP Town Hall, where we spent a considerable portion of our time debriefing APIC’s review and recommendations regarding ERAS alternatives.
CORD has decided to partner with ResidencyCAS to help us develop our own platform specifically designed to support our emergency medicine residency application process. This custom-built platform will streamline the entire application process for students, Program Directors, and Program Coordinators, while also reducing administrative and financial burdens, and will ultimately enhance the experience for everyone involved.
-
We understand that the announcement yesterday from ABEM concerning public access to Program Board pass rates has generated significant conversation and concern. The Board is committed to collaborating with ABEM as we move forward to advance our specialty through effective communication and cooperation. We look forward to our upcoming Town Hall at ACEP's Scientific Assembly, where we will engage in open dialogue about this and other important issues affecting Emergency Medicine.
Proudly serving you,
The CORD Board of Directors
-

Joint Statement on the Emergency Medicine 2024 Match Results
In the 2024 Match, we enthusiastically welcomed over 3000 new residents to Emergency Medicine!
Much has been said about the EM Match of the last 2 years. This year’s results are a testament to the resilience of our specialty, an acknowledgment of the critical role EM holds in the House of Medicine, and a result of dedicated work from many stakeholders. Our specialty thanks everyone for their hard work and dedication in recruiting our new and talented residents, who meet the mission and vision of our EM Programs.
Our EM organizations commit to building a supportive environment for current and future EM physicians. We all celebrate a tremendously successful EM Match and a bright future together in a specialty whose mission is to answer the call of “Anyone, Anything, Anytime.”
2023
-
CORD Support of DO Applicants
"In emergency medicine, a growing number of applicants have osteopathic backgrounds, constituting a robust and expanding segment of our medical community. CORD values osteopathic education, and osteopathic students merit equal opportunity as they apply for residency. CORD also recognizes undue barriers may exist for DO degree holders when applying to emergency medicine residency programs. In your evaluation of resident applicants, CORD encourages all programs to accept COMLEX-USA results as equivalent to the USMLE, ensuring equitable consideration for osteopathic applicants alongside their allopathic peers."
-
CORD Support of Christus Spohn
CORD recently learned of the unexpected closing of our member program Christus Spohn, located in Corpus Christi, TX, effective June of 2026.
We wanted to share our support for their Program Director, Dr. Alainya Tomanec and her 36 residents, along with a few details that we know to be true.
CORD supports and stands with the Program Director and her leadership team. As of the date of the announcement, Dr. Tomanec has been in her position for a mere 90 days. We are humbled and impressed with Dr. Tomanec’s dedication to her residents, as she remains in place supporting them. We all empathize with the stress and anxiety of learning the PD job, but to have to close your Program so quickly upon assuming this leadership role is unprecedented.
-
Joint Statement from Emergency Medicine Organizations on Efforts to Diversify Health Care Professionals in the United States
Following the recent U.S. Supreme Court decisions on the consideration of an applicant's racial or ethnic background in the higher education admissions process, our emergency medicine organizations stand together in our efforts to diversify health care professionals, including physicians, in the United States.
Additionally, we reaffirm our responsibility to addressing health care disparities and inequities as we deliver exceptional care to all patients who enter our emergency departments.
-
2023 CORD Statement on Residency Interviews
Emergency Medicine has a diverse landscape of programs, each with unique needs and goals. It is our intent to promote the balance that exists between program autonomy, student access to programs, and advocacy for the well-being of our members by providing guidance for programs regarding the 2023-2024 recruitment season.
Our recommendation is to utilize a virtual interview format with the opportunity for in-person visits later in the season.
-
Joint Statement on the Emergency Medicine 2023 Match Results
Each year the emergency medicine (EM) community celebrates Match week, as we welcome another group of talented EM residents to our specialty.
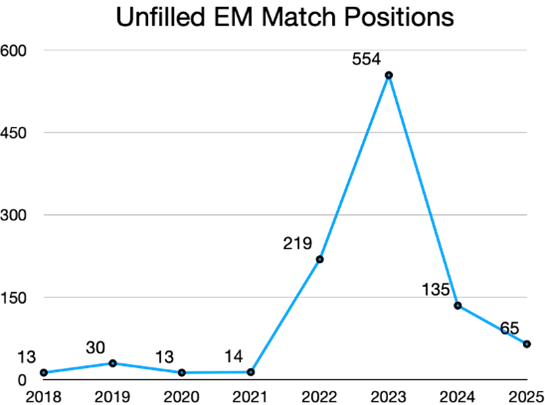
The 2022 EM Match saw an unprecedented initial 219 unmatched positions affecting one in four residency programs. The 2023 Match will see 555 initially unmatched positions, affecting a larger number of residency programs. Although these are challenging results, EM remains a vibrant and appealing specialty for many with almost 2500 new trainees already joining the EM family.
2022
-
Multi-Organizational Letter Regarding AHRQ Report on Diagnostic Errors in the Emergency Department
As experts in emergency medicine, our organizations are committed to improving patient care in the practice of emergency medicine. Yet, we are deeply concerned about the recently released report and systematic review by Dr. David Newman-Toker, et. al., entitled Diagnostic Errors in the Emergency Department: A Systematic Review. This work was conducted through an Evidence-Based Practice Center (EPC) as part of AHRQ’s Effective Health Care Program. After reviewing the executive summary and initial draft, we believe that the report makes misleading, incomplete, and erroneous conclusions from the literature reviewed and conveys a tone that inaccurately characterizes and unnecessarily disparages the practice of emergency medicine (EM) in the United States (U.S.).
-
Statement on Applicant Numbers for EM Residency Positions
ERAS just released the first round of data on residency applicants. This information has confirmed everyone’s suspicions that applications to emergency medicine residency have dropped substantially. This decrease of 20% over last year comes on the heels of the challenging 2022 match which left 69 of our 277 programs with 219 open slots to fill.
Potential explanations for this decrease are multifactorial. They may include reactions to the recent EM workforce study1, increasing levels of emergency physician burnout,2 and the highly visible challenges of coping with ubiquitous boarding and mental health crises. CORD will continue to engage with follow-up research for the workforce group as additional publications have questioned the assumptions underlying the original projections.3,4
-
Dear Colleagues,
It has come to our attention that Doximity is, once again, working to create “reviews” of emergency medicine residency training programs with biased, opinion-based methodology. This flawed data approach does not benefit students applying to emergency medicine or emergency medicine residency programs.
The emergency medicine specialty organizations’ previous letters (dating back to 2014) have had no response nor resulted in the cessation of the Doximity crowd-sourced, review-culture survey. Doximity is again publicizing this survey, encouraging emergency medicine physicians to participate.
As the leadership in the specialty, we strongly oppose the Doximity survey and cannot recommend emergency physicians participate and students use or be influenced by flawed research methodology.
-
Dear CORD Collective,
Over the past several months we, your Board of Directors, have been involved with ongoing conversations about the upcoming recruitment season format. Clearly this is an issue of utmost importance that affects us all.
It is our goal to promote the balance that exists between program autonomy, student access to programs, and advocacy for the wellbeing of our members by providing guidance regarding the 2022-23 recruitment season. Recognizing the diversity of opinions and needs as well as the potential for unanticipated challenges with COVID, we have intentionally structured these as recommendations rather than requirements.
We are grateful for your participation, feedback, and the wide range of preferences that you shared in the survey. The data we gathered from our membership (124 responses) indicates majority support (70%) for one singular format but there is mixed support for each format, 29.8% support in person interviews, 25.8% support virtual, and 40.3% support a hybrid of virtual interviews with in person second looks.
-
Consensus Statement for the Emergency Medicine 2022-2023 Residency Application Cycle Regarding Emergency Medicine Away Rotations
The COVID-19 pandemic created unique challenges for medical students, clerkship directors, program directors, and student advisors related to multiple aspects of the residency application process. Due to pandemic-related restrictions, the Coalition for Physician Accountability (CoPA) has issued guidelines on these topics for the past two application seasons. The Emergency Medicine (EM) community has subsequently released specific recommendations for applicants to our specialty (1-3). This year, CoPA is not issuing updated guidelines and as a result, there remains ambiguity and variability in advising practices regarding emergency medicine rotations including away rotations (4).
To address this and the need for formalized guidance, the above organizations have developed consensus guidelines related to expectations for emergency medicine rotations based on the best available evidence and practices. The purpose of this statement is to provide clarity about this particular aspect of the application process and to optimize equity and consistency. An additional intent is to recognize these rotations as valuable finite resources and assure they are available to all applicants pursuing EM residency training (5). Students need a minimum of one Standardized Letter of Evaluation (SLOE) to apply to emergency medicine. Two SLOEs are preferred by many programs. These guidelines apply to the Main Residency Match and do not apply to students who have contractual obligations with the military or are applying to the military match.
We recognize that there is not a one-size-fits-all model and there are certain groups of students who may need additional rotations.
-
Joint Statement on the 2022 Emergency Medicine Residency Match
Each year, the National Resident Matching Program is an exciting, yet anxious time for those involved. Together, we enthusiastically welcome the 2,702 newly matched residents into the emergency medicine family and commit to supporting each of our nation’s future emergency physicians.
Coupled with our excitement is some concern regarding a few of the results from the 2022 Main Residency Match. While emergency medicine remains in the Top 10 for match rates, according to the NRMP, our specialty had 219 unfilled positions in the 2022 Match - a more than 7 percentage point increase from last year. (These numbers do not include the Supplemental Offer and Acceptance Program (SOAP), and complete data from that program will be available at a later date.)
2021
-
Joint Statement on the EM Workforce
Our specialty has been working for decades to meet the growing emergency medicine needs of our country. The recent research is critical to identifying and understanding the challenges we face about the future workforce for both academic and community emergency physicians.Market consolidation, fragmentation and health care economics have shifted incentives across our industry. On top of these trends, the COVID-19 pandemic exposed many vulnerabilities within the health care system and accelerated concerns for our recent residency graduates.
As emergency physicians, it is our nature to want solutions quickly, but we must respond thoughtfully with a data-driven, forward-looking approach. As the leading organizations of Emergency Medicine, we will continue to work together to monitor the supply and demand of emergency care. We will continue to test the assumptions and forecasts in the predictive modeling, especially as we emerge from the COVID-19 pandemic. And we will develop this critical data into an action plan to broaden and redefine emergency medicine.
We know Emergency Medicine is a critical specialty -- one with a bright and promising future. Emergency medicine will continue to evolve to provide the best possible care for our patients in this rapidly changing healthcare environment. We are committed to working with all partners in this critical endeavor to mitigate current and anticipated impacts to our profession at every stage.
-
Recommendations on Program-Sponsored Events During the 2021-2022 Interview Season
The Coalition for Physician Accountability (CoPA) recently released recommendations for the 2021-2022 interview season for postgraduate training. In summary, the Coalition recommends that all interviews should be conducted virtually. This recommendation was made based on the growing incidence of COVID-19 variants as the pandemic continues to pose a threat to public health.
The Coalition recommendation was designed to promote equity among applicants and programs during the entirety of the interview season.
Given the unanswered questions from applicants and programs about potential recruitment season events (such as second looks and social events) in light of the CoPA statement, the Clerkship Directors in Emergency Medicine (CDEM), the Council of Residency Directors in Emergency Medicine (CORD-EM), and the Emergency Medicine Residents’ Association (EMRA) came to consensus on all interview season activities for the 2021-2022 emergency medicine application cycle.
We consider any events where representatives from the program (faculty or residents) participate with applicants to be program-sponsored events. This includes in-person visits to the residency program or with its representatives, site visits to the institution, and meetings or social events with residency leaders, faculty, or residents. We consider all in-person program-sponsored events to be inconsistent with the CoPA recommendations for an all-virtual interview season. As such, we endorse the following:
- All emergency medicine residency interviews should be conducted virtually.
- In-person program-sponsored events should not occur during the 2021-2022 interview season.
- Virtual visits for “second looks” are acceptable.
- Applicants may independently choose to visit a city as part of their decision-making process during the 2021-2022 interview season, but they should not request to participate in, nor should they be offered in-person program-sponsored events.
Offering in-person program-sponsored events would not only jeopardize public health but also undermine equity in the application process. Applicants may feel pressure to attend in-person events if offered, and those who are unable to do so for health or financial reasons may be placed at a real or perceived disadvantage relative to their peers. Institutional restrictions and/or local COVID-19 prevalence may prevent some programs from offering in-person events, placing them at a disadvantage relative to those who are able to offer such events. It is in the interest of equity that we support the CoPA recommendation for a virtual interview season and believe that this guidance must extend to all interview season activities.
-
Consensus Statement on the 2021-2022 Emergency Medicine Residency Application Cycle Part I: Emergency Medicine Rotations and Letters
On January 25, 2021, the Coalition for Physician Accountability (CoPA) released guidelines regarding away rotations for students participating in the upcoming residency application cycle in light of the ongoing COVID-19 pandemic. The primary recommendations were:
- No away rotations before 8/1/2021, except for students with a specialty interest they are unable to pursue at their home institutions
- Tentative resumption of away rotations after 8/1/2021, with a limit of one such rotation per student
As a field that relies heavily on away rotations, Emergency Medicine (EM) is uniquely affected by these recommendations. The purpose of this statement is to affirm conceptual support for the CoPA guidelines and to describe the specifics of how they should be operationalized in EM to optimize equity and consistency in the residency application process. An additional intent is to recognize these rotations as valuable finite resources and assure they are available to the majority of applicants. In light of the continually changing landscape of the pandemic, this statement will be re-evaluated as new information becomes available, and will be revised if needed in May 2021. These guidelines apply to the Main Residency Match and do not apply to students who have a contractual obligation to the military or are applying to the military match.
In an effort to promote safety, fairness, and equity in the EM residency application process, we strongly recommend the following principles be followed:- The timelines outlined by CoPA for away rotations should be followed by all institutions offering EM rotations.
- EM residency applications should include a maximum of two electronic Standardized Letters of Evaluation (eSLOEs).
- The mechanism by which students receive their two eSLOEs will vary according to individual circumstances.
- Students without access to an EM rotation at their home institution should be considered and prioritized for these limited away rotation spots.
- We strongly encourage EM leaders to forge partnerships with medical schools in their regions that do not host EM residency programs, with the goal of providing a “home” for students who would otherwise lack access to home rotations.
- Away rotations should not be required or expected for this application year for students with access to a “home” rotation
- The intent of these recommendations is to assure they are available to the majority of applicants
- Vaccination status should not be used as a determinant of rotation eligibility. S
- Students should follow all institutional, local, state, and federal guidelines in planning their rotations.
-
CORD is deeply saddened and angered by anti-Asian violence across the country. We are committed to using our voice and platform to speak up against racism. We stand with our Asian, Asian-American, Pacific Islander communities and all BIPOC communities affected by racism, sexism, and exclusionary constructs.
We want to take this opportunity to underscore our commitment to you, and our esteemed faculty, residents, and students, as we promote a safe and equitable learning environment in our training programs and in our larger communities. In addition to supporting you in your academic missions, we will not rest in the fight to end structural racism, sexism, discrimination, and all other unacceptable constructs, until they are eradicated.
As leaders, we owe it to our trainees to be role models and speak out. We stand together in the fight for antiracism, diversity, inclusion, and respect for all persons. Moving forward will mean, at times, working through seemingly unfathomable circumstances and situations that cause us pain. Let us remember our strength and resolve as a community, and be quick to share love and support to those who need it.
CORD’s vision is for a future with opportunity, equity, and peace for all. In the meantime, we shall lean on each other and look forward to a better day.
Proud to serve, Your CORD Board of Directors
-
We are watching with you as the situation at the Tulane University campus is currently unfolding. We were shocked to read the details of the allegations, and can only imagine the strength it takes to come forward in the circumstances that Dr. Dennar describes in the lawsuit.
While CORD is not in the position to comment on the ongoing investigation, we do want to take this opportunity to underscore our commitment to you, and our esteemed faculty, residents, and students, as we promote a safe and equitable learning environment in our Training Programs.
In addition to supporting you in your academic missions, we will not rest in the fight to end structural racism, sexism, discrimination, and all other unacceptable constructs, until they are eradicated. We support zero-tolerance policies, and as leaders, we owe it to our trainees to be role models and speak out.
We stand together in the fight for antiracism, diversity, inclusion, and alongside every individual and group who has faced a similar fight, big or small. Moving forward will mean, at times, working through seemingly unfathomable circumstances and situations that cause us pain. Let us remember our strength and resolve as a community, and be quick to share love and support to those who need it.
We hope that the outcomes in this case, and others like it, will bring opportunity, equity, and peace in the future. In the meantime, we shall lean on each other and look forward to a better day.
Proud to serve,
Your CORD Board of Directors
2020
-
The entire Emergency Medicine community, as represented by the undersigned organizations, is disheartened to see recent comments and national news stories that might confuse the public about the training and scope of practice of osteopathic physicians and emergency medicine specialists.
Doctors of Osteopathic Medicine (DOs) make up a substantial segment of the fully licensed practicing physicians in the US. DOs complete the same years of medical school as MDs, earning state licenses to practice the full scope of medicine and surgery and entering the same pathways to residency in all specialties in the US.
This year 27.4% of physicians entering emergency medicine training were graduates of U.S. Osteopathic schools and hence have the degree DO after their names. Osteopathic physicians practicing Emergency Medicine serve in all health care settings including rural, urban, and military. Osteopathic physicians have served as military Surgeon General, and multiple emergency physicians have served as the physician to the president.
Over 42,000 emergency physicians, both MDs and DOs, are distinctly trained, certified, and uniquely qualified to lead teams of multi-disciplinary professionals working together to make the best decisions possible for their patients. These tireless front line professionals stand on the front lines, day in and day out, in all of the emergency departments in the US and worldwide, 24 hours a day, 7 days a week, 365 days a year. With gratitude, we proudly stand in support of all practicing emergency physicians - both DO and MDs-and ask that our support and solidarity be widely disseminated to educate the public.
-
It has come to our attention that Doximity is, once again, surveying emergency physicians to create “rankings” of emergency medicine residency training programs with a biased methodology. This type of flawed data approach does not benefit students applying to emergency medicine or emergency medicine residency programs, all of whom are working diligently to provide excellent physician training. As we have declared before, our specialty organizations strongly oppose Doximity’s approach to ranking programs.
In 2014, the emergency medicine specialty organizations signed a joint letter to Dr. Gross from Doximity with no response or cessation of the Doximity survey. Doximity is publicizing this survey again in 2020, encouraging emergency medicine physicians to participate. Doximity is recommending their survey results to students as valid data to assist them in making application and ranking decisions. We, as the leadership in the specialty, strongly oppose the Doximity survey, recommending that emergency physicians not participate in the survey and recommend to students not be influenced by flawed research methodology.
As noted in 2014, we are concerned about the sampling method chosen for this survey, because we believe it will fail to achieve the objective for this survey— to identify America’s top emergency medicine training programs. Asking only physicians enrolled in a social media website to nominate their most preferred residencies will result in egregious sample bias and is not capable of resulting in a scientifically valid result. The results will be based solely upon opinions expressed by physicians who have no first-hand knowledge of any residency training programs other than the ones they attended themselves.
“While not a formal ranking of residency programs, the results would convey that some programs provide better training than others. However, given the limitations, this would not be an accurate portrayal— to medical students or to the public. It also would not be useful to many medical students, because research shows that more than 75 percent of emergency physician residents report the number one reason for selecting a residency program is geography.
“More concerning, the results could send a dangerous public health message to people with medical emergencies. It implies they should consider bypassing hospital emergency departments with residency programs that fared poorly in the survey. In a medical emergency, people should seek emergency care at the nearest emergency department, not one that scored better on a highly subjective opinion survey.
Patients need confidence in their physicians in times of crisis, especially since comparison shopping among doctors is not an option when someone is having a medical emergency. Emergency medicine residency programs train physicians in the emergent and acute conditions of just about every medical specialty in health care. As a result, emergency physicians are uniquely qualified to handle a full range of adult and pediatric emergencies. In addition, they see every kind of human drama imaginable, often treating multiple patients at a time.
The overall quality of medical care delivered in emergency departments in the United States is excellent, thanks to the uniformly high standards that govern the accreditation of residency programs in emergency medicine. Emergency medicine residencies collaborate openly with shared curricular tools built around a core model of clinical practice, an approach that is fairly unique in medical education. Ranking training programs above others is contrary to the principles of our specialty, although we recognize that certain programs are best suited for certain trainees.
“Many factors contribute to a successful residency program, not all of which can be measured or compared.”
The current COVID-19 pandemic has created more challenges for both residency leadership and students applying to residency. Promoting such a subjective survey does not benefit our specialty, students applying to our specialty, or residency training programs in emergency medicine, or the patient’s and communities we serve. We have offered Doximity’s team to create an improved survey with more valid methodology but did not receive a response. We understand that Doximity’s CEO, Jeff Tangney, has, more recently, not responded to emails from emergency medicine physicians asking for Doximity to cease conducting this survey.
Our specialty organizations represent over 40,000 thousand physicians.
We strongly oppose participation in the current survey by emergency physicians.
We strongly oppose encouraging the use of the Doximity survey data by medical students applying to emergency medicine residency programs as a factor in their selection.
-
The undersigned representatives of Emergency Medicine physicians are unified in their support of physician-led patient care and training. Although all who provide care in the Emergency Department setting must be appropriately trained, education of emergency medicine resident physicians and medical students must not be compromised or diluted. The terms “resident,” “residency,” “fellow,” and “fellowship” in a medical setting must be limited to postgraduate clinical training of medical school physician graduates within GME training programs. Physicians must lead patient care teams and actively shape standards for education and scope of practice of non-physician providers. Hospitals or employers should not create or advertise post-graduate training of nurse practitioners or physician assistants in the emergency department without explicit involvement and approval of the emergency medicine departmental and residency leadership.
-
The Council of Residency Directors in Emergency Medicine (CORD) appreciates this opportunity to share our position on faculty protected time with the ACGME. Substantial faculty non-clinical contributions are required to sustain graduate medical education. Residency programs are charged with providing crucial specialty training that encompasses both on-the-job supervision and separate didactic education outside of the clinical environment. Ultimate responsibility for residency training within the program lies primarily with the program director, assistant/associate program director(s), and program coordinator(s). These individuals carry a heavy administrative burden; without sufficient support, the demands of the job can become overwhelming and consuming, leading to burnout and job turnover. 1,2,3,4 Core faculty also play an essential role in fulfilling the educational and administrative functions of the graduate medical education. 5 Supported time for program administration and resident education serves as the buttress for academic faculty who engage in the non-clinical work that allows residency programs to successfully train residents and meet accreditation standards.
-
The American College of Emergency Physicians (ACEP), the American Academy of Emergency Medicine (AAEM), the American Academy of Emergency Medicine Resident and Student Association (AAEM/RSA), the Emergency Medicine Residents' Association (EMRA), the Council of Residency Directors in Emergency Medicine (CORD) and the Society for Academic Emergency Medicine (SAEM) recognize the growing evidence regarding the efficacy of facial coverings in combination with other measures to decrease the spread of COVID-19. We believe that the emergency department is not the proper setting for requesting or providing excuses from mask compliance.
-
The American Board of Emergency Medicine (ABEM) and the American Osteopathic Board of Emergency Medicine (AOBEM) will now provide letters of support that may be submitted to hospital credentialers to forego the need for additional short courses or certifications in the use of Emergency Ultrasound by emergency physicians. Physicians must be participating in the ABEM continuing certification process or the AOBEM Osteopathic Continuous Certification Program to obtain the letter.
The letter, signed by the ABEM, AOBEM, American Academy of Emergency Medicine, American Academy of Emergency Medicine/Resident and Student Association, American College of Osteopathic Emergency Physicians, Association of Academic Chairs of Emergency Medicine, Council of Residency Directors in Emergency Medicine, Emergency Medicine Residents’ Association, and Society for Academic Emergency Medicine, such as the Focused Assessment with Sonography in Trauma (FAST) examination; the determination of the presence of cardiac activity and/or pericardial effusion; or, to assist with placement of central venous access catheters. ABEM-certified physicians can download the letter from their Personal Page on the ABEM secure portal (instructions). AOBEM-certified physicians can obtain a letter upon request to AOBEM.
2019
-
To the Association of American Medical Colleges (AAMC),
As representatives of the Emergency Medicine community, we write today to communicate that our organizations do not support further study or use of the Standardized Video Interview (SVI).
We understand that the number of applications per applicant to Emergency Medicine programs has doubled over the past decade, (1) and that this has increased pressure on residency programs to screen which students to invite for in-person interviews. We applaud the AAMC for proactively identifying a potential gap in the residency application process with the 2016 Program Director Survey, (2) for being willing to innovate the residency application process, and for collaborating with representative bodies within the Emergency Medicine community.
However, after 3 years of piloting the SVI, reviewing the data, and hearing from the members of our community, we respectfully oppose further study or use of the SVI. Specifically, our position is based upon:
- Lack of evidence to support SVI
The SVI was intended to address the fact that Program Directors report a lack of adequate tools to assess an applicant’s interpersonal and communications skills and professionalism.2 However, after 3 years of data collection, the SVI has not been demonstrated to be the tool to fill this gap. Specifically, evidence shows that evaluation of professional and interpersonal communication skills by Emergency Medicine faculty during in-person interviews significantly differs from SVI scores.3 The Emergency Medicine community has yet to see conclusive data correlating SVI scores to outcome metrics, such as reaching ACGME milestones. Together, these data cast doubt upon the ability of the SVI to achieve its intended aim of improving the residency application process. - Uncertainty around cost
After 3 years of study, the AAMC is unable to provide information regarding the costs of the SVI, and if implemented, who would bear these costs. We are concerned about the potential financial burden this might place upon applicants and/or programs. Additionally, we are concerned about the indirect costs of SVI preparation that students may feel pressured to incur. For example, only 22% of applicants in a recent survey reported being provided a professional recording space to record their SVI, and one SVI preparation service charges $497 - $2,997.(4,5) - Student perceptions
The SVI was intended to benefit applicants by providing them the opportunity to feel holistically reviewed, (6) but only 31% of students agreed that the SVI would help program directors conduct a more holistic evaluation.(5) Additionally, less than one quarter of applicants agreed that the SVI gave them an opportunity to describe their interpersonal and communication skills or knowledge of professional behavior, and only half agreed that they were able to answer SVI questions based upon past experiences.5 Furthermore, more than half of applicants were satisfied with program director use of USMLE Step 1 and Step 2 CK scores as filters in the residency selection process (55% and 64%, respectively), while only 10% were satisfied with SVI as a filter.5 The majority of medical students are open to a variety of innovations, such as regional in-person interviews and live video interviews with programs.(5)
Moving Forward
While we do not support continued study or use of the SVI, we applaud the AAMC for attempting to innovate and improve the residency application process.
The Emergency Medicine community recognizes that interpersonal and communication skills as well as professionalism are critical competencies for Emergency Physicians and difficult to remediate competencies.7,8 Program directors still need and encourage objective standards of measurement for medical students in these competencies. The SVI project should highlight to all those working with medical students that there is a concerning lack of standardization between medical schools in how they assess their students.9 This lack of standardization in assessments creates opportunities for bias and lack of parity between student cohorts which raises significant concerns for both program directors and medical
students.
We are glad to have supported a project that highlighted how valuable our community holds the competencies of interpersonal and communication skills and professionalism. As we move past the SVI pilot project, we look forward to continuing to collaborate to improve the residency application process together. - Lack of evidence to support SVI
-
A joint policy statement of the American College of Emergency Physicians, American Academy of Emergency Medicine, American Academy of Emergency Medicine Resident and Student Association, American Board of Emergency Medicine, American College of Osteopathic Emergency Physicians Graduate Medical Education Committee, American Osteopathic Board of Emergency Medicine, Association of Academic Chairs of Emergency Medicine, Council of Emergency Medicine Residency Directors, Emergency Medicine Residents’ Association, Society for Academic Emergency Medicine, and the Society for Academic Emergency Medicine Resident and Medical Students
Emergency medicine is unique in that it provides 24-hour clinical care for a diverse range of high-acuity, life-threatening illnesses and requires direct, continuous, on-site faculty supervision of residents. Because a substantial portion of residency education consequently occurs outside the domain of regular clinical shifts, protection of core faculty educational time is essential. Core faculty have been defined as those faculty who work clinically and devote the majority of their professional efforts to emergency medicine graduate medical education (GME).1 Program leadership and core faculty are critical to the success of the training missions of emergency medicine residency and fellowship programs. Core faculty require compensated time to engage in necessary residency education, administration, and scholarly activities outside of the clinical environment; without protected time for core faculty to accomplish this, the quality of emergency medicine residency training and clinical care may decline. At a minimum, all emergency medicine core faculty should be allocated protected time per the 2017 Accreditation Council for Graduate Medical Education (ACGME) Emergency Medicine Common Program Requirements: emergency medicine core faculty clinical hours should be limited to no more than 28 hours per week or 1344 hours per year, whichever is fewer.1
1. Program Requirements for GME in Emergency Medicine – ACGME [Internet]. Program Requirements for GME in Emergency Medicine – ACGME. 2017 [cited 2019 Feb 27]; Available from: https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/110_emergency_medicine_2017-07-01.pdf
2017
-
Founded in 1989, the Council of Emergency Medicine Residency Directors (CORD) has served to promote the free exchange of ideas and solutions to challenges faced by Emergency Medicine educators. CORD has long recognized that supporting our educators and trainees goes far beyond professional and academic resources and associations. In this capacity, CORD was formed also with the goal of developing a close-knit community of clinician educators and program coordinators for the purpose of providing a personal and supportive community of practice.
To further support and expand upon the founding values of CORD, in 2015 the Resilience Committee was formed with the purpose of focusing on the wellbeing of our residents and educators. The goals of the committee are to:
- Promote a culture of wellness among faculty and residents.
- Develop best practices for resilience and coping techniques during residency.
- Establish a strategy to support residency programs that have had residents or faculty die by suicide.
- Provide curricular resources on wellness and long-term career satisfaction.
- Establish a network for faculty and residents interested in advancing wellness in emergency medicine.
- Promote research and scholarship in wellness.
Since its inception, the Resilience Committee has been able to achieve several milestones for promoting well-being within the Emergency Medicine education community, including: ongoing collaborative efforts with the American Foundation for Suicide Prevention and the Take 5 to Save Lives Campaign; establishing a continually updated database of Wellness Champions at institutions across the country; creating modules and curricula for residency programs on wellness topics; developing best practices for assessing resident wellness; inspiring collaborative research efforts between institutions; and innovating wellness training programs for residents.
CORD is fully committed to addressing the professional and personal issues which lead to EM physician unwellness within academic medicine as well as promoting practices at all levels of administration that support EM physician well-being for lifelong practice.
-
CORD firmly believes that the independent practice of emergency medicine (EM) is best performed by graduates from emergency medicine residency training programs. Successful completion of an EM residency program accredited by the Accreditation Council for Graduate Medical Education (ACGME) or American Osteopathic Association (AOA) is the criterion standard. Emergency medicine physicians who may practice independently are eligible to take or have successfully passed the American Board of Emergency Medicine (ABEM) or the American Osteopathic Board of Emergency Medicine (AOBEM) certification.
-
The American Board of Emergency Medicine(ABEM)defines the standards for the specialty of Emergency Medicine. Certification by ABEM supersedes the need for any additional certifications sometimes required for medical staff privileges or disease-specific care center designations, such as that needed for trauma or stroke centers. Herein, ABEM and supporting Emergency Medicine organizations oppose any requirement of additional short courses or topic-specific continuing education for ABEM and AOBEM-certified emergency physicians, who are in good standing with their medical staff, and who are participating in Maintenance of Certification, or Osteopathic Continuous Certification, or any future program to ensure continued Board Certification.
Emergency Medicine organizations provide high quality opportunities for continuous professional development in advanced resuscitation, trauma care, stroke care, cardiovascular care, procedural sedation, pediatric care, and airway management.
The knowledge, skills, and abilities needed for the care of the acutely ill and injured are sufficiently described in The Model of the Clinical Practice of Emergency Medicine (EM Model), and are ensured by obtaining and maintaining ABEM certification. The EM Model is the foundational document for designing an Emergency Medicine residency curriculum, and is also the document on which ABEM bases the content of its initial certification and continuous certification (ConCert™) examinations. Residency training in the Model and subsequent oral and written assessments are far more rigorous than any of the topic-specific continuing education courses (i.e., ACLS, PALS, ATLS, etc.)
An ABEM-certified physician has successfully passed a secure, comprehensive written examination that includes questions about airway management, pharmacotherapy, cardiovascular care, and trauma care with an emphasis on critical and emergent conditions. If the physician successfully passes the written examination, she or he must then take an oral examination. The ABEM Oral Certification Examination is a highly reliable test that requires the physician to demonstrate the diagnostic evaluation and treatment of complex clinical conditions.
The ABEM Maintenance of Certification Program is a rigorous program of continuous professional development that contains content critical to the practice of Emergency Medicine. The ConCert™ Examination is a high-stakes, psychometrically valid, secure, and comprehensive examination weighted toward high acuity conditions. The ABEM Maintenance of Certification program includes content pertaining to procedural sedation, cardiovascular care, airway management, trauma care, stroke management, and pediatric acute care. For the Lifelong Learning and Self-Assessment (LLSA) test requirement, ABEM-certified emergency physicians are required to read 10-15 articles for each test yearly. The content and rigor of the ABEM LLSA requirements exceed the knowledge and skills that could be gained from any of the aforementioned short courses.
ABEM-certified physicians who are active in the ABEM Maintenance of Certification program should not be required to obtain additional certification or content-specific educational requirements. For physicians who are not board certified in Emergency Medicine, completion of periodic, short courses in focused content areas of Emergency Medicine may be valuable. Nonetheless, additional short courses or certifications are unnecessary for ABEM and AOBEM-certified emergency physicians.
2016
-
CORD’s formal position on the current ACGME resident duty hour requirements, including impact analysis, from CORD’s perspective, on costs and impact of implementation.
- CORD supports the concept of resident duty hour requirements to promote a supportive educational environment with resident well-being and patient safety.
- CORD has concerns about the effect of resident duty hour requirements on patient safety, transitions of care, quality of training and costs.
- CORD believes resident duty hours should be revised to better support the educational experience for trainees.
- CORD recommends that the ACGME should establish specialty-specific duty hour requirements for all specialties.
CORD’s formal recommendations regarding dimensions of resident duty hours requirements, and justification (wherever possible) for these recommendations with evidence.
- CORD supports duty hours that will enhance patient safety and resident wellness.
- CORD recommends the ACGME provide more flexibility in duty hours to provide for resident scheduling flexibility and professional development.
- CORD recommends absolving residency programs of monitoring external moonlighting hours.
- CORD recommends revising duty hours to promote professional citizenship, patient accountability and academic service.
2014
-
- The term “Emergency Physician” should only be used to refer to one of the following:
- Graduates of ACGME- or AOA-accredited Emergency Medicine residency programs who are ABEM or AOBEM board eligible or board certified.
- Those physicians who completed training in another specialty and who received ABEM or AOBEM certification before the closure of the practice pathways and are currently certified by either of those bodies; and physicians who applied through the practice pathways before their closure and are currently designated as board eligible by ABEM or AOBEM.
- Graduates of ACGME- or AOA-accredited programs in pediatrics who also completed a Pediatric Emergency Medicine fellowship that was accredited by the ACGME or AOA.
- Retired physicians who met the above definitions during their careers.
- The term “Emergency Medicine Resident Physician” should only be used to refer to current resident physicians serving in an ACGME/AOA accredited Emergency Medicine Residency working in an emergency department as part of their education.
- Fellows in an ACGME- or AOA-accredited Pediatric Emergency Medicine fellowship working in an emergency department as part of their education are “Pediatric Emergency Medicine Fellow Physicians.”
- Physicians who have not met the above criteria and who practice in an Emergency Department should be identified as “(other specialty physician) providing emergency care”, “emergency care provider” or “physician working in the emergency department.”
BACKGROUND:Within the United States, Emergency Medicine is recognized as a specialty by the American Board of Medical Specialties (ABMS) and the American Osteopathic Association (AOA). Responsibilities of specialty status include accrediting graduate medical education training programs and credentialing physicians as certified specialists. In the U.S., Emergency Medicine training is accredited by the Accreditation Council for Graduate Medical Education Review Committee – Emergency Medicine (ACGME RC-EM), or the American Osteopathic Association Council on Postdoctoral Training – Emergency Medicine (AOA COPT-EM). The primary Emergency Medicine certifying bodies in the U.S. are the American Board of Emergency Medicine (ABEM) and the American Osteopathic Board of Emergency Medicine (AOBEM). In the case of Pediatric Emergency Medicine, the American Board of Pediatrics (ABP) is recognized as an ABMS certifying body in pediatrics, which provides a Certificate of Special Qualifications for pediatricians in the subspecialty of Pediatric Emergency Medicine.It is the role and responsibility of ABEM and AOBEM to contribute to the training standards, assess competency through board certification processes and establish professional practice principles for Emergency Physicians.CORD has consistently maintained that Emergency Medicine is best learned through residency training unique to the specialty with proof of initial competence to enter unrestricted practice of medicine through educational assessment and passage of either the ABEM or AOBEM certification examination.Residents in training or other physicians who do not meet these criteria are less likely to possess the cognitive and technical skill set necessary for rendering unsupervised care for the tremendous breadth and acuity of situations encountered in an ED.Many outstanding physicians contributed to the creation of Emergency Medicine into an independent medical specialty. These physicians are recognized for their dedication and unique role in our specialty’s history.Approved by the Board of Directors: March 31, 2013 - The term “Emergency Physician” should only be used to refer to one of the following:
2013
-
The Council of Emergency Medicine Residency Directors (CORD) believes that emergency medicine (EM) residents should receive training regarding conflicts of interest that may arise from the promotion and marketing efforts of industry, primarily the pharmaceutical industry. These conflicts may arise between pharmaceutical company representatives and any of the targets of their marketing, including physicians, nurses, and patients. Furthermore, EM residents should be instructed in critical appraisal methods so that unbiased judgments can be made regarding the efficacy of industry products. Residency programs should create policies that guide residents in dealing with pharmaceutical company representatives, potential conflicts of interest, and acceptable resolutions of these conflicts. CORD strongly supports the Accreditation Council for Graduate Medical Education (ACGME) white paper on the relationship between graduate medical education and industry and encourages its adoption by members.
Received May 9, 2003; accepted May 20, 2003. Address for correspondence: Sam Keim, MD: sam@aemrc.arizona. edu; or Debra G. Perina, MD: dgp3a@hscmail.mcc.virginia.edu. A related article appears on page 19. doi:10.1197/S1069-6563(03)00591-8
-
Emergency Medicine residency directors are faced with an ever-expanding breadth of knowledge and skills to teach in their curriculum. Over the last decade the number of "Advanced Life Support" courses (ATLS, ACLS, APLS, PALS, NALS) has continued to grow. Mandated attendance of such courses has proven problematic from both a time and a financial standpoint. In addition, the information may not be as up to date or applicable as the program director would like. Our graduates continue to encounter mandated certification in order to join medical staffs or obtain ED clinical privileges, an archaic practice dating to the days when untrained practitioners were the norm in the ED.
The CORD Board of Directors has developed two position statements addressing Advanced Life Support courses referenced above. The first applies to our graduates as they seek medical staff appointments or clinical privileges. The second addresses our teaching institutions in which mandated attendance may be encountered as a prerequisite for our EM residents’ participation in a clinical training venue.
Graduates:
The CORD believes that Emergency Department patient care is best provided by specialists who have successfully completed an accredited residency program in Emergency Medicine. Such individuals are trained to a much more rigorous standard than found in such courses. For this reason, CORD recommends that such courses not be required for medical staff appointments or clinical privileges for ABEM/ABOEM certified or EM residency trained physicians.
Teaching Institutions:
There has been a proliferation of Advanced Life Support Courses and certification, with content applicable to EM. The course contents are routinely taught to EM residents as a portion of their core curriculum in EM. For this reason, CORD does not support mandated attendance or certification as a prerequisite for participation in selected clinical residency requirements or rotations. The appropriate preparation for such curriculum elements is best determined on a local level by the EM residency director.
These position statements should not be interpreted as a blanket condemnation of all Advanced Life Support Courses. Program directors may choose to examine the course content on a case by case basis for their less experienced EM residents, and decide if the course fits their curriculum needs.
-
CORD believes that ED patient care is best provided by specialists who have successfully completed an accredited residency program in emergency medicine. Residents should not engage in the independent practice of emergency medicine.
-
CORD believes that resident safety is of paramount importance in all training settings and that an air medical experience may place residents at higher risk. CORD believes that emergency medicine residents must understand air medical transportation of patients including selection, EMS medical direction, flight capability and safety, and flight physiology and CORD recognizes that some programs have established an area of excellence in this training. CORD does not believe that flight experience is required to gain an adequate level of understanding. Programs that do request or allow residents to fly on rotary aircraft should be certain that the aircraft are certified and maintained according to the highest standards promulgated by the appropriate credentialing boards. Programs should also ensure that residents are educated into the risks of air medical transport prior to their first flight.
-
- CORD members and their staff should consider all written electronic communications from applicants to be confidential and not for distribution beyond the program personnel involved in resident selection unless permission is granted by applicant.
- The dissemination of negative information about an applicant to outside parties is improper unless contained in a letter of recommendation or in response to a direct question from another program.
- Any serious concerns regarding professionalism, related to an applicant may be brought to the attention of the Dean of Student Affairs at the applicant's school with a request that the Dean investigate the matter and notify as appropriate the programs the applicant has sent their information to.
-
CORD receives many requests for assistance with, and support for, sponsorship, or endorsement of surveys of emergency medicine residency programs. Therefore, the CORD Board has developed the following guidelines: As the organization representing all emergency medicine program directors, CORD is uniquely qualified to assist in the performance of surveys relating to resident education. CORD's Board of Directors will consider requests from the membership for sponsorship of surveys and research projects involving program directors, residents or other related groups. The decision to sponsor, support, or endorse a project will be based upon the following guidelines:
As the organization representing all emergency medicine program directors, CORD is uniquely qualified to assist in the performance of surveys relating to resident education. CORD's Board of Directors will consider requests from the membership for sponsorship of surveys and research projects involving program directors, residents or other related groups. The decision to sponsor, support, or endorse a project will be based upon the following guidelines:
1. Surveys and/or projects should be developed by committees or task forces of the organization and should be consistent with their overall goals.
2. Surveys and projects may be sponsored either independently or in conjunction with other emergency medicine organizations. If joint sponsorship with another organization is desirable, it is the responsibility of the project developers to apply for appropriate support, endorsement, or sponsorship from that organization.
3. Requests for sponsorship, support, or endorsement of a proposed survey should be submitted in writing to the Board of Directors. Requests should include a brief description of the rationale for the proposed survey and the perceived benefit to the organization or its membership. A detailed budget should describe costs related to printing, mailing, data analysis and publication as well as any other expenses associated with the project. A copy of the survey or research instrument should also accompany the request for sponsorship, support, or endorsement.
4. Task forces or committees receiving sponsorship, support, or endorsement will be expected to issue a follow-up report to the Board of Directors and the membership. When appropriate, publication in a peer-reviewed journal is desirable.
5. Credit for authorship of published research results should be based upon accepted principles governing authorship of scientific publications. CORD's sponsorship of published survey results should be noted in the acknowledgments accompanying publications.
6. The CORD listserv is not the appropriate venue to post the survey, the Sharepoint IS the appropriate and best method to distribute or post surveys for CORD member participation, and a brief email to the listserv announcing the posting on Sharepoint is permitted. Sharepoint will have a section for CORD endorsed survey and research instruments, and a separate section for brief, non-CORD endorsed surveys.
Advocacy
-
Dream Act Health Professionals Statement of Support
Health professional organizations have come together to support legislation that would provide a pathway to citizenship for undocumented young people and those approved for Deferred Action for Childhood Arrivals (DACA)
-
Coalition to Oppose Medical Merit Badges
Earlier this year, in partnership with all of the major Emergency Medicine (EM) organizations, CORD was proud and honored to support an initiative opposing medical institutions that require board certified EM physicians to: (1) maintain certification in various resuscitation courses, and (2) to have mandatory short-course continuing medical education for various subspecialty areas such as stroke and trauma.
Like many of the other EM initiatives of which CORD has been a part, we believe that by banding together, we can continue to advance our specialty by speaking with one voice. The following letter is being sent on behalf of the CORD Board of Directors. -
Joint Organization letter regarding VA Policy
Out of Operating Room Airway Management (OORAM) Certification for non-anesthesiologists - Letter to Veterans Administration
-
CORD Response Letter to ACGME regarding Duty Hours
-
Joint Organization letters regarding Doximity Medical Student Survey
-
CORD Response to ACGME Proposed Revisions to Duty Hours
The ACGME has proposed revisions to the common program requirements for resident duty hours
-
CORD Recommendations for revising the ABEM Policy on Credit for Prior Training
CORD was asked to offer recommendations for revising the ABEM policy on credit for prior training
-
NRMP Policy Change